In Australia, the use of medicinal cannabis has grown rapidly since its legalisation for medical purposes in 2016. With more than 320,000 Special Access Scheme (SAS) approvals granted by late 2022 and over 800 cannabis products available, general practitioners and authorised prescribers face a complex and evolving landscape. A comprehensive medicinal cannabis database plays a crucial role in supporting evidence-based prescribing, maintaining TGA compliance, and improving patient outcomes.
Why General Practitioners Need More Medicinal Cannabis Knowledge
Australian general practitioners are often the first point of contact for patients seeking medicinal cannabis for chronic conditions such as pain, anxiety, or sleep disorders. However, many clinicians report limited knowledge about medicinal cannabis and its therapeutic applications. In a 2020 study, nearly 67% of surveyed GPs felt their knowledge was inadequate, while only 22% had prescribed cannabis.
This highlights the need for centralised, accurate information on cannabis as medicine. Unlike conventional drugs, medicinal cannabis products differ greatly in cannabinoid content, form (oil, capsule, dried flower), and clinical indications. Prescribers must navigate both clinical uncertainty and regulatory requirements.
What is a Medicinal Cannabis Database?
A medicinal cannabis database or knowledge base is an organised collection of medicinal cannabis products with detailed information, tailored for practitioners. Practitioners can use the medicinal cannabis database to find and learn about different medicinal cannabis products, to help when issuing prescriptions for their patients.
Why Comprehensive Databases Matter
A dedicated medicinal cannabis database offers multiple benefits for authorised prescribers:
1. Product Clarity
Databases provide up-to-date listings of all TGA-notified medicinal cannabis products. This helps doctors compare options by THC/CBD content, form, category, and more. Since most products are unregistered and require SAS or Authorised Prescriber (AP) approval, knowing the correct category (e.g., Category 1 for CBD-only) is essential for compliance.
2. Evidence-Based Guidance
Databases link to clinical guidelines and systematic reviews on cannabis for medical conditions. This enables prescribers to evaluate the medical literature and assess the benefits of medicinal cannabis for conditions like epilepsy, chronic pain, and nausea. Such resources help address the gap in formal training and support safe prescribing practices.
3. Simplified Regulatory Navigation
Prescribing under the SAS or AP scheme involves documentation and understanding of TGA rules. A cannabis database can offer templates, checklists, and alerts about regulatory updates. This ensures prescribers stay compliant and avoid delays or errors.
4. Safety and Dosing Information
Knowing how to titrate doses and anticipate side effects (e.g., sedation or cognitive impairment from THC) is vital. A database can summarise this data, improving patient safety and guiding doctors in tailoring medicinal cannabis use to each patient’s needs.
5. Improved Patient Access
Doctors with access to reliable data can confidently choose suitable products and access pathways. This shortens the time from consultation to prescription fulfilment, improving patient access and treatment outcomes.
Addressing Prescriber Concerns
Despite growing interest in prescribing medicinal cannabis, many practitioners remain cautious. Concerns include a lack of standardised dosing, potential side effects, and insufficient evidence for some indications. A well-structured database helps bridge this knowledge gap.
By centralising clinical guidance and public health updates, the database empowers practitioners to make informed decisions and counsel patients effectively. It distinguishes between medical use and recreational cannabis use, reinforcing the therapeutic intent of prescribed cannabis.
Enhancing Clinical Outcomes
Comprehensive databases improve:
- Decision-making: Matching symptoms (e.g., chronic pain) to appropriate cannabis formulations.
- Consultation quality: Offering accurate answers about product effects, safety, and access.
- Compliance: Ensuring prescriptions align with TGA approvals and product categories.
- Consistency: Promoting uniform practices across prescribers.
These factors contribute to improved patient satisfaction and clinical outcomes. As more doctors feel supported in their practice, access to medicinal cannabis expands in a responsible and regulated manner.
The Path Forward
With attitudes of Australian general practitioners towards medicinal cannabis becoming more positive, the demand for reliable resources is rising. A comprehensive database provides a vital foundation for safe, informed prescribing. It supports doctors in:
- Navigating the regulatory system (SAS/AP)
- Understanding cannabis and cannabinoids
- Accessing product-specific clinical data
- Supporting best practices in medical cannabis treatment
By integrating data, guidelines, and access tools, such a database transforms cannabis prescribing from a niche challenge into a standardised medical process. It enhances prescriber knowledge, patient safety, and public trust in the use of cannabis for medical treatment.
Conclusion
Medicinal cannabis prescribing in Australia is no longer a fringe activity. With demand increasing and the benefits of medicinal cannabis becoming clearer, doctors need dependable resources. A comprehensive database streamlines prescribing, strengthens clinical decision-making, and ensures compliance with TGA standards. For medical practitioners, it’s an essential tool in delivering effective, personalised care in the era of cannabis medicine.
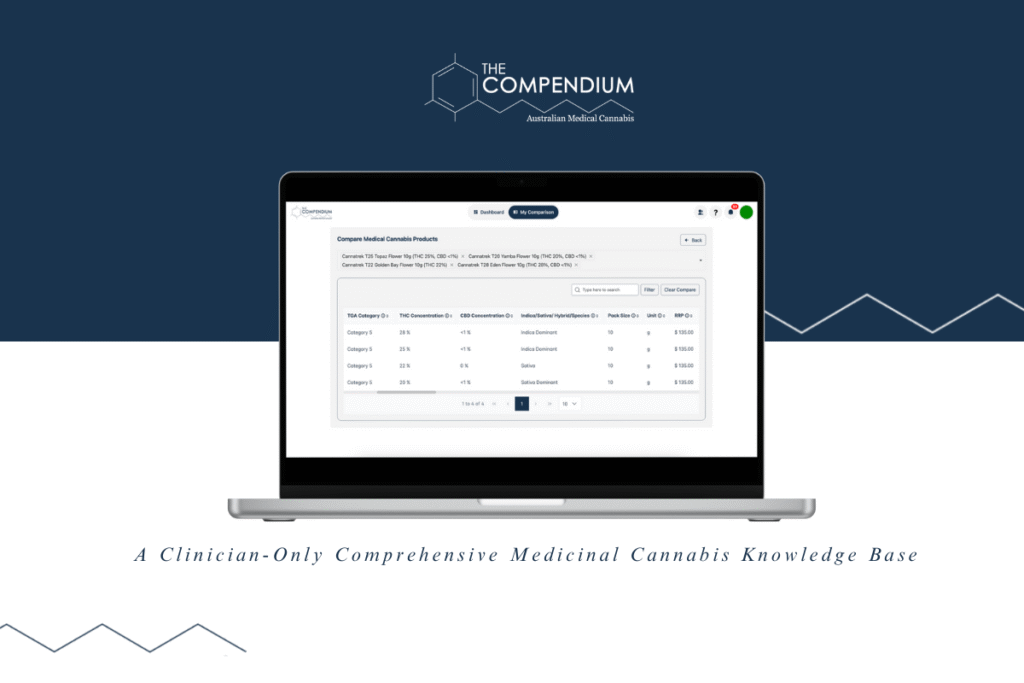
The Compendium provides authorised prescribers with a dedicated, clinician-focused database that bridges the gap between clinical practice and regulatory demands. Whether you’re navigating the Special Access Scheme or seeking evidence-based insights for patient treatment plans, The Compendium offers the clarity, compliance, and confidence required for modern cannabis prescribing.
Start prescribing with confidence. Explore The Compendium today and empower your cannabis clinical practice.

