Why Prescribing Medicinal Cannabis Requires Precision
Prescribing medicinal cannabis in Australia has become increasingly common, but it’s a space that demands caution, knowledge, and adherence to strict guidelines. With growing access to medicinal cannabis and a wider range of therapeutic goods available, the role of the clinician has never been more crucial.
Unfortunately, many well-meaning medical practitioners fall into avoidable traps that can compromise patient outcomes, regulatory compliance, and their professional reputation. Here are the most common mistakes clinicians make when prescribing medicinal cannabis and, importantly, how to avoid them.
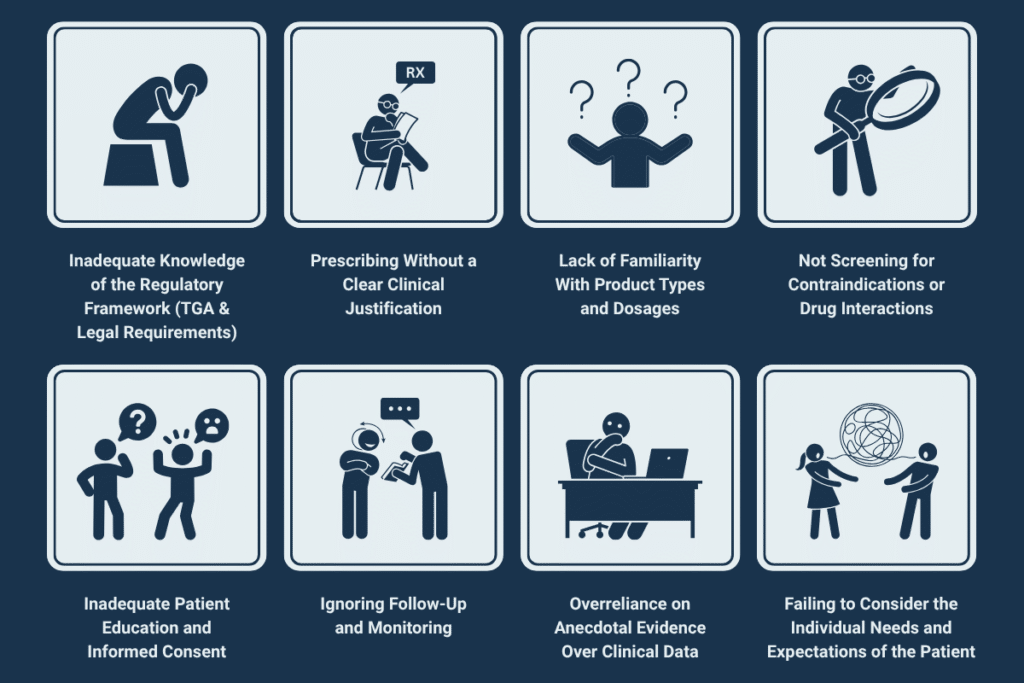
1. Inadequate Knowledge of the Regulatory Framework (TGA & Legal Requirements)
Many clinicians underestimate the importance of staying up to date with the Therapeutic Goods Administration (TGA) guidelines. The TGA regulates all prescriptions of medicinal cannabis in Australia, requiring applications via the Special Access Scheme (SAS) or Authorised Prescriber Scheme.
Avoid it by:
- Regularly reviewing TGA updates and clinical guidance: https://www.tga.gov.au/medicinal-cannabis-guidance-documents
- Completing Continuing Medical Education (CME) on medicinal cannabis prescribing
- Consulting legal resources on the current legislation in your state or territory
2. Prescribing Without a Clear Clinical Justification
Medicinal cannabis is not a first-line treatment. Clinicians must demonstrate that conventional therapies have been tried and found ineffective or unsuitable before prescribing medical cannabis.
Avoid it by:
- Documenting the patient’s medical condition and previous treatment history
- Clearly articulating why medicinal cannabis may benefit this patient
- Using validated treatment protocols supported by medical research
3. Lack of Familiarity With Product Types and Dosages
Not all medicinal cannabis products are the same. Some contain only cannabidiol (CBD), others tetrahydrocannabinol (THC), and some are combinations. Inappropriate product choice or dosing can lead to adverse effects or a lack of therapeutic benefit.
Avoid it by:
- Understanding the effects of medicinal cannabis formulations (CBD-dominant vs. THC-dominant)
- Starting low and going slow with dosing
- Choosing from the medicinal cannabis products available in Australia based on TGA-approved references
4. Not Screening for Contraindications or Drug Interactions
Medicinal cannabis can interact with other medications (e.g., anticoagulants, antidepressants) and may not be suitable for patients with a history of psychosis, cardiovascular disease, or substance use disorders.
Avoid it by:
- Conducting thorough patient histories and medication reviews
- Screening for psychiatric risk factors or comorbidities
- Consulting drug interaction databases before prescribing
5. Inadequate Patient Education and Informed Consent
Patients using medicinal cannabis need to understand the legal, clinical, and lifestyle implications, especially when it comes to driving, workplace testing, and potential side effects.
Avoid it by:
- Explaining the benefits and risks in clear, non-technical language
- Documenting informed consent discussions
- Providing printed or digital materials on medicinal cannabis use
6. Ignoring Follow-Up and Monitoring
Medicinal cannabis treatment is not a set-and-forget prescription. Effects may change over time, and patients may misuse or discontinue treatment without guidance.
Avoid it by:
- Setting regular follow-up appointments
- Monitoring for side effects, efficacy, and adherence
- Using patient feedback to adjust treatment where necessary
7. Overreliance on Anecdotal Evidence Over Clinical Data
While patient stories and peer experiences are helpful, they are no substitute for peer-reviewed medical research and clinical guidelines.
Avoid it by:
- Relying on systematic reviews, clinical trials, and guidance from bodies like the National Health and Medical Research Council (NHMRC)
- Accessing reputable databases such as PubMed or government-sponsored portals
For example, a 2022 study by the Australian Institute of Health and Welfare found that over 70,000 Australians accessed prescribed medicinal cannabis through legal channels, with patients self-reporting improvements in chronic pain and anxiety symptoms.
8. Failing to Consider the Individual Needs and Expectations of the Patient
Each patient’s perception of medicinal cannabis and its effects can vary. Some may expect instant results or have misconceptions about how it works.
Avoid it by:
- Clarifying that medicinal cannabis is a treatment, not a cure
- Discussing realistic timelines and goals
- Involving patients in shared decision-making
Elevating Patient Outcomes Through Responsible Prescribing
Prescribing medical cannabis in Australia is a promising yet complex field. Avoiding these common pitfalls not only ensures safer patient outcomes but also strengthens the legitimacy of medicinal cannabis in the treatment landscape.
At The Compendium, we help clinicians navigate the ever-evolving world of medicinal cannabis with evidence-based resources, expert insights, and continuing medical education.
Ready to enhance your prescribing confidence with evidence-based tools? Contact us today to access professional tools and clinical support.

